Natural malaria infection elicits rare but potent neutralizing antibodies to the blood-stage antigen RH5.
Wang, L.T., Cooper, A.J.R., Farrell, B., Miura, K., Diouf, A., Muller-Sienerth, N., Crosnier, C., Purser, L., Kirtley, P.J., Maciuszek, M., Barrett, J.R., McHugh, K., Ogwang, R., Tucker, C., Li, S., Doumbo, S., Doumtabe, D., Pyo, C.W., Skinner, J., Nielsen, C.M., Silk, S.E., Kayentao, K., Ongoiba, A., Zhao, M., Nguyen, D.C., Lee, F.E., Minassian, A.M., Geraghty, D.E., Traore, B., Seder, R.A., Wilder, B.K., Crompton, P.D., Wright, G.J., Long, C.A., Draper, S.J., Higgins, M.K., Tan, J.(2024) Cell 187: 4981-4995.e14
- PubMed: 39059381
- DOI: https://doi.org/10.1016/j.cell.2024.06.037
- Primary Citation of Related Structures:
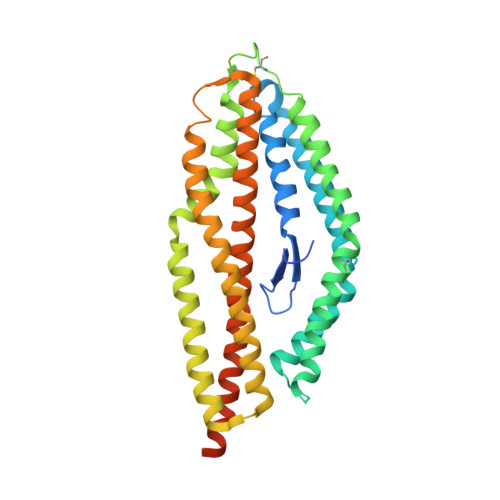
8PWU, 8PWV, 8PWW, 8PWX, 8Q5D - PubMed Abstract:
Plasmodium falciparum reticulocyte-binding protein homolog 5 (RH5) is the most advanced blood-stage malaria vaccine candidate and is being evaluated for efficacy in endemic regions, emphasizing the need to study the underlying antibody response to RH5 during natural infection, which could augment or counteract responses to vaccination. Here, we found that RH5-reactive B cells were rare, and circulating immunoglobulin G (IgG) responses to RH5 were short-lived in malaria-exposed Malian individuals, despite repeated infections over multiple years. RH5-specific monoclonal antibodies isolated from eight malaria-exposed individuals mostly targeted non-neutralizing epitopes, in contrast to antibodies isolated from five RH5-vaccinated, malaria-naive UK individuals. However, MAD8-151 and MAD8-502, isolated from two malaria-exposed Malian individuals, were among the most potent neutralizers out of 186 antibodies from both cohorts and targeted the same epitopes as the most potent vaccine-induced antibodies. These results suggest that natural malaria infection may boost RH5-vaccine-induced responses and provide a clear strategy for the development of next-generation RH5 vaccines.
- Antibody Biology Unit, Laboratory of Immunogenetics, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, MD 20852, USA; Vaccine Research Center, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD 20892, USA; Department of Biochemistry, University of Oxford, South Parks Road, Oxford OX1 3QU, UK; Medical Scientist Training Program, University of California, San Diego School of Medicine, La Jolla, CA 92093, USA.
Organizational Affiliation: